FL in pregnancy stands for Femur Length, which is a crucial measurement taken during routine ultrasounds to assess the growth and development of the fetus. FL is an important indicator of fetal well-being and can provide valuable information about the gestational age and potential abnormalities. As a pregnant woman, understanding what FL is and its significance can help you monitor your baby’s progress and ensure a healthy pregnancy.
In this article, we will provide a comprehensive guide on FL in pregnancy, including its definition, measurement, and interpretation, to help you stay informed and empowered throughout your pregnancy journey.
What Is FL In Pregnancy?
FL in pregnancy refers to Femur Length, which is a measurement taken during ultrasound examinations of the developing fetus in the womb. The femur is the longest bone in the human body and is a key indicator of fetal growth and development.
During an ultrasound, a specialized machine uses high-frequency sound waves to produce images of the fetus. One of the measurements taken is the length of the femur bone, which is then used to estimate the gestational age of the fetus. This measurement is particularly important during the second trimester of pregnancy when fetal growth is most rapid.
FL can also be used to detect potential abnormalities or growth restrictions in the fetus. For example, if the FL measurement is consistently below average, it may indicate that the fetus is not growing as expected, which can be a sign of fetal growth restriction or other underlying medical conditions.
Overall, FL is an essential part of routine ultrasound examinations during pregnancy, providing valuable information about fetal growth and development, and helping healthcare providers monitor the health and well-being of both the mother and baby.
How FL Is Measured?
FL, or femur length, is a measurement used during pregnancy to evaluate fetal growth and development. It is one of the biometric parameters used to assess fetal size, along with other measurements such as head circumference, abdominal circumference, and biparietal diameter. FL is measured in millimeters from the endpoint of the femur (thigh bone) to the endpoint of the other femur, and it is typically measured during routine ultrasound examinations.
The FL measurement is important because it can provide important information about the fetal size and development, as well as the amount of amniotic fluid present in the uterus. This information can be used to detect and monitor fetal growth abnormalities, predict fetal weight, and identify other potential complications during pregnancy. In particular, FL measurement is useful for assessing the growth of fetuses with conditions such as fetal growth restriction, chromosomal abnormalities, and skeletal dysplasia.
In clinical practice, FL measurement is considered normal when it falls within a certain range based on the gestational age of the fetus. Abnormal FL measurements may indicate potential issues with fetal growth or development, and additional diagnostic tests and interventions may be necessary to evaluate and manage these issues.
There are several factors that can affect the accuracy of FL measurements. Technical factors such as the skill and experience of the sonographer, the quality of the ultrasound machine, and the position of the fetus can all impact the measurement. Fetal factors such as the fetal position and posture, the presence of abnormalities or anomalies, and fetal growth rate can also affect FL measurement accuracy. Additionally, maternal factors such as maternal obesity, diabetes, and hypertension can also influence the accuracy of FL measurements.
In summary, FL measurement is an important tool for evaluating fetal growth and development during pregnancy. It can provide valuable information that can help identify potential complications and facilitate appropriate management and care. However, it is important to be aware of the factors that can affect the accuracy of FL measurements and to take these factors into consideration when interpreting and using the measurement data.
Why Is FL Measured During Pregnancy?
Femur length (FL) is measured during pregnancy as part of routine ultrasound examinations. The FL measurement provides important information about fetal growth and development and is used to assess fetal size, predict fetal weight, and evaluate amniotic fluid volume. Here are some of the main reasons why FL is measured during pregnancy:
- Detection of fetal growth abnormalities: FL measurement is one of the biometric parameters used to evaluate fetal growth and development. Abnormal FL measurements may indicate potential issues with fetal growth or development, such as fetal growth restriction, which is a condition in which the fetus is smaller than expected for its gestational age.
- Prediction of fetal weight: FL measurement is also used to estimate fetal weight. This is important because it can help healthcare providers to anticipate potential complications during labor and delivery, such as macrosomia, a condition in which the baby is larger than average, which can increase the risk of complications such as shoulder dystocia.
- Evaluation of amniotic fluid volume: FL measurement is also used to evaluate the amount of amniotic fluid present in the uterus. This is important because too little or too much amniotic fluid can indicate potential complications such as oligohydramnios or polyhydramnios, respectively.
In clinical practice, FL measurement is considered normal when it falls within a certain range based on the gestational age of the fetus. Abnormal FL measurements may indicate potential issues with fetal growth or development, and additional diagnostic tests and interventions may be necessary to evaluate and manage these issues. Overall, FL measurement is an important tool for evaluating fetal growth and development during pregnancy and for ensuring the best possible outcomes for both mother and baby.
Detection Of Fetal Growth Abnormalities
Fetal growth abnormalities can occur during pregnancy, and detecting them early is essential for proper management and intervention. Femur Length (FL) is one of the fetal biometric measurements that can be used to identify potential growth abnormalities.
If the FL measurement is consistently below the expected range for the gestational age, it may indicate that the fetus is not growing as expected. This can be a sign of fetal growth restriction, which is a condition in which the fetus is not growing at the expected rate. Fetal growth restriction can be caused by various factors, such as maternal health conditions, placental insufficiency, or fetal genetic abnormalities.
On the other hand, if the FL measurement is consistently above the expected range, it may indicate that the fetus is growing too rapidly. This can be a sign of fetal macrosomia, a condition in which the fetus is larger than average for its gestational age. Fetal macrosomia can increase the risk of complications during delivery, such as shoulder dystocia or cesarean delivery.
Other fetal biometric measurements, such as head circumference, abdominal circumference, and biparietal diameter, are also used to identify potential growth abnormalities. When combined, these measurements can provide a comprehensive assessment of fetal growth and development.
If a potential growth abnormality is detected, further evaluation may be required, such as more frequent ultrasounds, fetal monitoring, or consultation with a specialist in maternal-fetal medicine. Early detection and management of fetal growth abnormalities can improve outcomes for both mother and baby, highlighting the importance of routine ultrasound examinations during pregnancy.
Prediction Of Fetal Weight
Fetal weight prediction is an important aspect of prenatal care, as it can help healthcare providers anticipate potential complications during labor and delivery. Fetal weight can be estimated using several methods, including ultrasound measurements such as femur length (FL) and abdominal circumference (AC), as well as other clinical factors such as maternal weight gain and gestational age.
One of the most commonly used ultrasound-based methods for predicting fetal weight is the Hadlock formula, which is based on measurements of AC, FL, and head circumference. The formula uses these measurements to estimate fetal weight in grams, taking into account factors such as the gestational age of the fetus and the sex of the baby.
FL measurement is a key component of the Hadlock formula, as it provides important information about fetal growth and development. FL measurement is typically obtained by measuring the length of the femur bone in millimeters during a routine ultrasound examination. The FL measurement is then used, along with other biometric parameters such as AC and head circumference, to estimate fetal weight using the Hadlock formula.
While fetal weight prediction can be useful for anticipating potential complications during labor and delivery, it is important to keep in mind that it is only an estimate and can be subject to a degree of error. Factors such as maternal obesity, fetal position, and growth rate can all affect the accuracy of fetal weight estimates. In addition, it is important to note that accurate fetal weight estimation is more difficult in certain situations, such as in cases of multiple gestation pregnancies or fetal anomalies.
Despite these limitations, fetal weight prediction based on FL measurement and other biometric parameters can provide valuable information for prenatal care and delivery planning. By working with healthcare providers to monitor fetal growth and development throughout pregnancy, expectant mothers can ensure the best possible outcomes for both themselves and their babies.
Evaluation Of Amniotic Fluid Volume
Amniotic fluid surrounds the developing fetus in the womb and plays a crucial role in fetal growth and development. The evaluation of amniotic fluid volume is an essential part of routine ultrasound examinations during pregnancy.
Amniotic fluid volume is evaluated using an ultrasound machine, which produces images of the fetus and the amniotic fluid. The amniotic fluid index (AFI) is one of the methods used to evaluate amniotic fluid volume. The AFI is calculated by measuring the depth of the amniotic fluid in four separate pockets in the uterus and adding the values together.
The AFI measurement can help identify potential issues with amniotic fluid volume, such as too much or too little fluid. Polyhydramnios is a condition in which there is too much amniotic fluid, while oligohydramnios is a condition in which there is too little amniotic fluid.
Polyhydramnios can be caused by various factors, such as gestational diabetes, fetal abnormalities, or twin-to-twin transfusion syndrome. Oligohydramnios can be caused by various factors, such as premature rupture of membranes, placental insufficiency, or fetal kidney problems.
If polyhydramnios or oligohydramnios is detected, further evaluation may be required, such as more frequent ultrasounds, fetal monitoring, or consultation with a specialist in maternal-fetal medicine. In some cases, delivery may need to be induced earlier than expected to reduce the risk of complications.
In summary, the evaluation of amniotic fluid volume is an essential part of routine ultrasound examinations during pregnancy. The AFI measurement can help identify potential issues with amniotic fluid volume, such as polyhydramnios or oligohydramnios. Early detection and management of these conditions can improve outcomes for both mother and baby, highlighting the importance of regular prenatal care and ultrasound evaluations.
How Is FL Measurement Used In Clinical Practice?
Femur length (FL) measurement is an important tool used in clinical practice during pregnancy to assess fetal growth and development. FL measurement is typically obtained during routine ultrasound examinations and is used for several purposes. Here are some of the ways that FL measurement is used in clinical practice:
- Evaluation of fetal growth: FL measurement is one of the biometric parameters used to assess fetal growth and development during pregnancy. Abnormal FL measurements may indicate potential issues with fetal growth or development, such as fetal growth restriction or macrosomia, which can affect the health of the baby and require further diagnostic tests or interventions.
- Prediction of gestational age: FL measurement is also used to predict gestational age. This is important because it can help healthcare providers to monitor fetal growth and development, anticipate potential complications, and adjust prenatal care accordingly.
- Estimation of fetal weight: FL measurement is one of the components used in fetal weight estimation formulas, such as the Hadlock formula, which is used to estimate fetal weight using ultrasound measurements of FL, abdominal circumference, and head circumference. Fetal weight estimation can help healthcare providers to anticipate potential complications during labor and delivery, such as macrosomia or shoulder dystocia.
- Detection of fetal anomalies: FL measurement can also be used to detect fetal anomalies, such as skeletal dysplasia, in which the fetal bones do not develop properly. Abnormal FL measurements, along with other ultrasound findings, can indicate potential fetal anomalies that require further diagnostic testing or intervention.
In clinical practice, FL measurement is considered normal when it falls within a certain range based on the gestational age of the fetus. Abnormal FL measurements may indicate potential issues with fetal growth or development, and additional diagnostic tests and interventions may be necessary to evaluate and manage these issues. Overall, FL measurement is an important tool for evaluating fetal growth and development during pregnancy and for ensuring the best possible outcomes for both mother and baby.
Normal Range Of FL Measurement
Femur Length (FL) is one of the fetal biometric measurements taken during routine ultrasound examinations of the developing fetus in the womb. The FL measurement is used to estimate the gestational age of the fetus and assess fetal growth and development.
The normal range of FL measurement can vary depending on the gestational age of the fetus. Generally, the FL measurement increases with gestational age. The average FL measurement at 14 weeks of gestation is about 2.5 cm, while the average FL measurement at 20 weeks of gestation is about 4.5 cm.
It is essential to note that FL measurement alone cannot be used to diagnose fetal growth abnormalities or gestational age. Other fetal biometric measurements, such as head circumference, abdominal circumference, and biparietal diameter, are also used to evaluate fetal growth and development.
The FL measurement can also be affected by various factors, such as fetal position, maternal body mass index (BMI), and fetal genetic abnormalities. Therefore, it is crucial to interpret the FL measurement in conjunction with other fetal biometric measurements and clinical information.
In summary, the normal range of FL measurement can vary depending on the gestational age of the fetus. The FL measurement is just one of several fetal biometric measurements used to evaluate fetal growth and development. It is important to interpret the FL measurement in conjunction with other fetal biometric measurements and clinical information to accurately assess fetal growth and development.
Abnormal FL Measurements And Their Implications
Abnormal femur length (FL) measurements during pregnancy can have implications for fetal growth and development. FL measurement is one of the biometric parameters used to assess fetal growth and development during pregnancy, and abnormal FL measurements may indicate potential issues that require further diagnostic testing or intervention. Here are some of the implications of abnormal FL measurements during pregnancy:
- Fetal growth restriction (FGR): Abnormally small FL measurements may indicate FGR, which is a condition in which the fetus is smaller than expected for its gestational age. FGR can lead to poor fetal outcomes, such as low birth weight and increased risk of neonatal morbidity and mortality. FGR may be caused by a variety of factors, such as placental insufficiency, maternal health conditions, or fetal genetic abnormalities.
- Macrosomia: Abnormally large FL measurements may indicate macrosomia, a condition in which the baby is larger than average. Macrosomia can increase the risk of complications during labor and delivery, such as shoulder dystocia, which can lead to birth injuries for both mother and baby. Macrosomia may be caused by factors such as maternal diabetes, maternal obesity, or fetal genetic abnormalities.
- Skeletal dysplasia: Abnormal FL measurements may also indicate skeletal dysplasia, a group of genetic disorders that affect the development of the fetal skeleton. Skeletal dysplasia can affect the size and shape of the fetal bones and may cause a range of health issues for the baby, such as breathing difficulties and skeletal abnormalities.
- Polyhydramnios or oligohydramnios: Abnormal FL measurements may also be associated with abnormalities in amniotic fluid volume. Polyhydramnios, a condition in which there is too much amniotic fluid, or oligohydramnios, a condition in which there is too little amniotic fluid, can have implications for fetal growth and development, and may require further diagnostic testing or intervention.
In cases of abnormal FL measurements, healthcare providers may recommend additional diagnostic tests or interventions, such as genetic testing, amniocentesis, or closer monitoring of fetal growth and development. The goal of these interventions is to identify any underlying issues that may be affecting fetal growth and development and to manage them appropriately to ensure the best possible outcomes for both mother and baby.
Additional Diagnostic Tests And Interventions
In some cases, additional diagnostic tests and interventions may be necessary to evaluate fetal growth and development during pregnancy. These tests and interventions can help identify potential issues and allow for appropriate management and treatment.
Some of the additional diagnostic tests that may be recommended include:
- Non-stress test (NST): This test measures the fetal heart rate in response to fetal movements. It is used to assess fetal well-being and can help identify potential issues such as fetal distress.
- Biophysical profile (BPP): This test combines the results of an NST with an ultrasound evaluation of fetal breathing, movements, tone, and amniotic fluid volume. It is used to assess fetal well-being and can help identify potential issues such as fetal distress.
- Doppler ultrasound: This test measures blood flow in the umbilical artery, which can provide information about placental function and fetal well-being.
- Amniocentesis: This test involves inserting a needle through the abdomen into the amniotic sac to obtain a sample of amniotic fluid. It can be used to diagnose genetic abnormalities, fetal lung maturity, or infection.
In addition to diagnostic tests, interventions may be necessary to manage potential issues with fetal growth and development. Some of the interventions that may be recommended include:
- Delivery: If a potential issue with fetal growth and development is identified, delivery may need to be induced or scheduled earlier than expected to reduce the risk of complications.
- Fetal monitoring: This involves monitoring the fetal heart rate and other fetal biometric measurements more frequently to assess fetal well-being and identify potential issues.
- Maternal medication: In some cases, medication may be recommended to improve blood flow to the placenta or treat maternal health conditions that can affect fetal growth and development.
In summary, additional diagnostic tests and interventions may be necessary to evaluate fetal growth and development during pregnancy. These tests and interventions can help identify potential issues and allow for appropriate management and treatment. It is important to work closely with a healthcare provider and follow their recommendations for optimal maternal and fetal health.
Factors That Can Affect FL Measurement Accuracy
Technical Factors
When measuring femur length (FL) during pregnancy, there are several technical factors that can affect the accuracy and reliability of the measurement. Here are some of the technical factors to consider when measuring FL:
- Gestational age: The accuracy of FL measurement is highly dependent on the gestational age of the fetus. FL measurements should be taken at the appropriate gestational age based on the expected due date to ensure accurate assessment of fetal growth and development.
- Fetal position: The position of the fetus can also affect FL measurement accuracy. For example, a breech presentation may affect the visibility of the fetal femur and make it more difficult to obtain an accurate measurement.
- Image quality: The quality of the ultrasound image is also important for accurate FL measurement. A clear image with good resolution and contrast can help to ensure that the fetal femur is properly identified and measured.
- Angle of measurement: The angle of measurement can also affect the accuracy of FL measurement. The femur should be measured at a 90-degree angle to ensure that the entire length of the bone is included in the measurement.
- Operator technique: The skill and technique of the ultrasound operator can also affect the accuracy of FL measurement. Proper training and experience can help to ensure that FL measurements are taken correctly and consistently.
- Equipment calibration: The calibration of the ultrasound equipment can also affect the accuracy of FL measurement. Regular calibration and maintenance of the equipment can help to ensure that measurements are accurate and reliable.
In order to obtain accurate and reliable FL measurements, it is important to consider these technical factors when performing ultrasound examinations during pregnancy. This can help to ensure that FL measurements are consistent, accurate, and useful for assessing fetal growth and development.
Fetal Factors
Fetal factors can play a significant role in fetal growth and development during pregnancy. These factors can include genetic abnormalities, fetal malformations, and fetal health conditions.
Genetic abnormalities can affect fetal growth and development by altering the expression of genes that control fetal growth. Some genetic abnormalities that can affect fetal growth include Down syndrome, Turner syndrome, and Trisomy 18.
Fetal malformations, such as congenital heart defects or neural tube defects, can also affect fetal growth and development. These malformations can affect the development of vital organs and systems, leading to issues with fetal growth and development.
Fetal health conditions, such as fetal anemia or fetal infections, can also impact fetal growth and development. These conditions can affect the ability of the fetus to obtain adequate oxygen and nutrients from the placenta, leading to issues with fetal growth and development.
It is important to identify and manage fetal factors that may impact fetal growth and development during pregnancy. This may involve additional diagnostic tests, such as amniocentesis or fetal echocardiography, to diagnose potential fetal health conditions or malformations. In some cases, fetal interventions, such as in-utero blood transfusions or fetal surgery, may be necessary to manage potential issues with fetal growth and development.
In summary, fetal factors can play a significant role in fetal growth and development during pregnancy. Genetic abnormalities, fetal malformations, and fetal health conditions can all impact fetal growth and development. It is important to identify and manage potential fetal factors to optimize maternal and fetal health.
Maternal Factors
Maternal factors can also play a role in femur length (FL) measurement during pregnancy. These factors can affect the accuracy of the measurement and may impact fetal growth and development. Here are some maternal factors to consider when measuring FL:
- Maternal height: Maternal height can affect FL measurement, as taller women tend to have larger fetal bones. When assessing FL measurements, it is important to take into account the mother’s height and adjust for any potential differences.
- Maternal weight: Maternal weight can also impact FL measurement accuracy. Maternal obesity, in particular, can make it more difficult to obtain accurate ultrasound images and may affect the ability to visualize the fetal femur.
- Maternal medical conditions: Certain maternal medical conditions, such as gestational diabetes or hypertension, can affect fetal growth and development and may impact FL measurements. It is important to consider any maternal medical conditions when interpreting FL measurements and to take appropriate steps to manage any potential complications.
- Maternal age: Maternal age can also impact fetal growth and development, as older mothers may be at increased risk for complications such as gestational diabetes or preeclampsia. These conditions can affect FL measurement accuracy and may require closer monitoring of fetal growth and development.
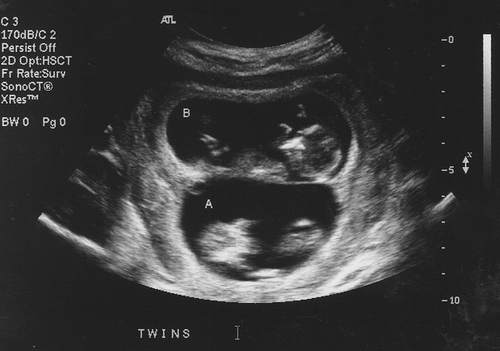
- Multiple pregnancies: In cases of multiple pregnancies, such as twins or triplets, FL measurement can be more challenging. The presence of multiple fetuses can make it more difficult to accurately visualize and measure each fetal femur.
- Amniotic fluid volume: Maternal factors can also affect amniotic fluid volume, which can impact FL measurement accuracy. Polyhydramnios or oligohydramnios can affect fetal growth and development and may require further diagnostic testing or intervention.
When assessing FL measurements during pregnancy, it is important to consider these maternal factors in order to obtain accurate and reliable measurements. Healthcare providers should take these factors into account when interpreting FL measurements and managing any potential complications related to fetal growth and development.
Conclusion
In conclusion, Femur Length (FL) is a crucial measurement taken during ultrasound examinations of the developing fetus during pregnancy. The femur bone is the longest bone in the human body and is an essential indicator of fetal growth and development. FL measurement is particularly important during the second trimester of pregnancy when fetal growth is most rapid.
FL is not only used to estimate the gestational age of the fetus, but it can also provide valuable information about potential abnormalities or growth restrictions. If the FL measurement is consistently below average, it may indicate that the fetus is not growing as expected, which can be a sign of fetal growth restriction or other underlying medical conditions. Hence, monitoring FL during routine ultrasound examinations is essential to identify any potential issues that may affect the health of the fetus and mother.
It is crucial for pregnant women to understand the significance of FL in pregnancy and the importance of routine ultrasound examinations. By staying informed and educated about the FL measurement, pregnant women can play an active role in monitoring their baby’s growth and development and ensure a healthy pregnancy.
Finally, it is worth noting that the measurement of FL is just one of many assessments done during routine ultrasound examinations, and its interpretation must be done in conjunction with other fetal biometric measurements and clinical findings. Therefore, it is essential to consult with a qualified healthcare provider for a complete evaluation of your pregnancy and ensure the best possible outcome for both mother and baby.



